About the lab
Cancer is a highly complex disease, and tumour progression requires the concerted action (and inaction) of many physiological systems. To survive, tumours co-opt and modify many different biological processes. This can happen both locally in the tumour’s immediate area, its ‘microenvironment’, and more widely across the whole organism, its ‘macroenvironment.’ In doing so, cancer affects normal physiology in ways that can be detrimental and often fatal for patients.
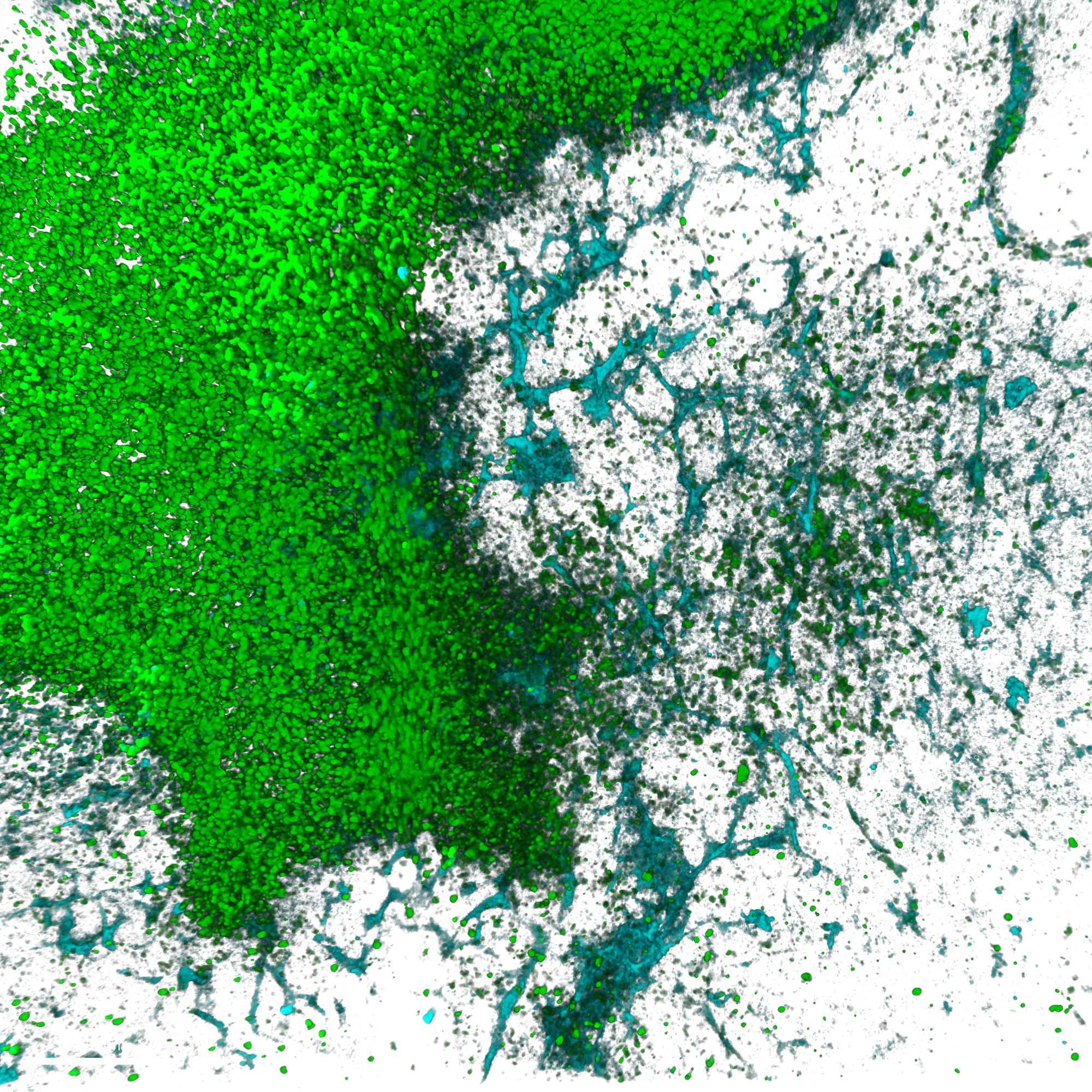
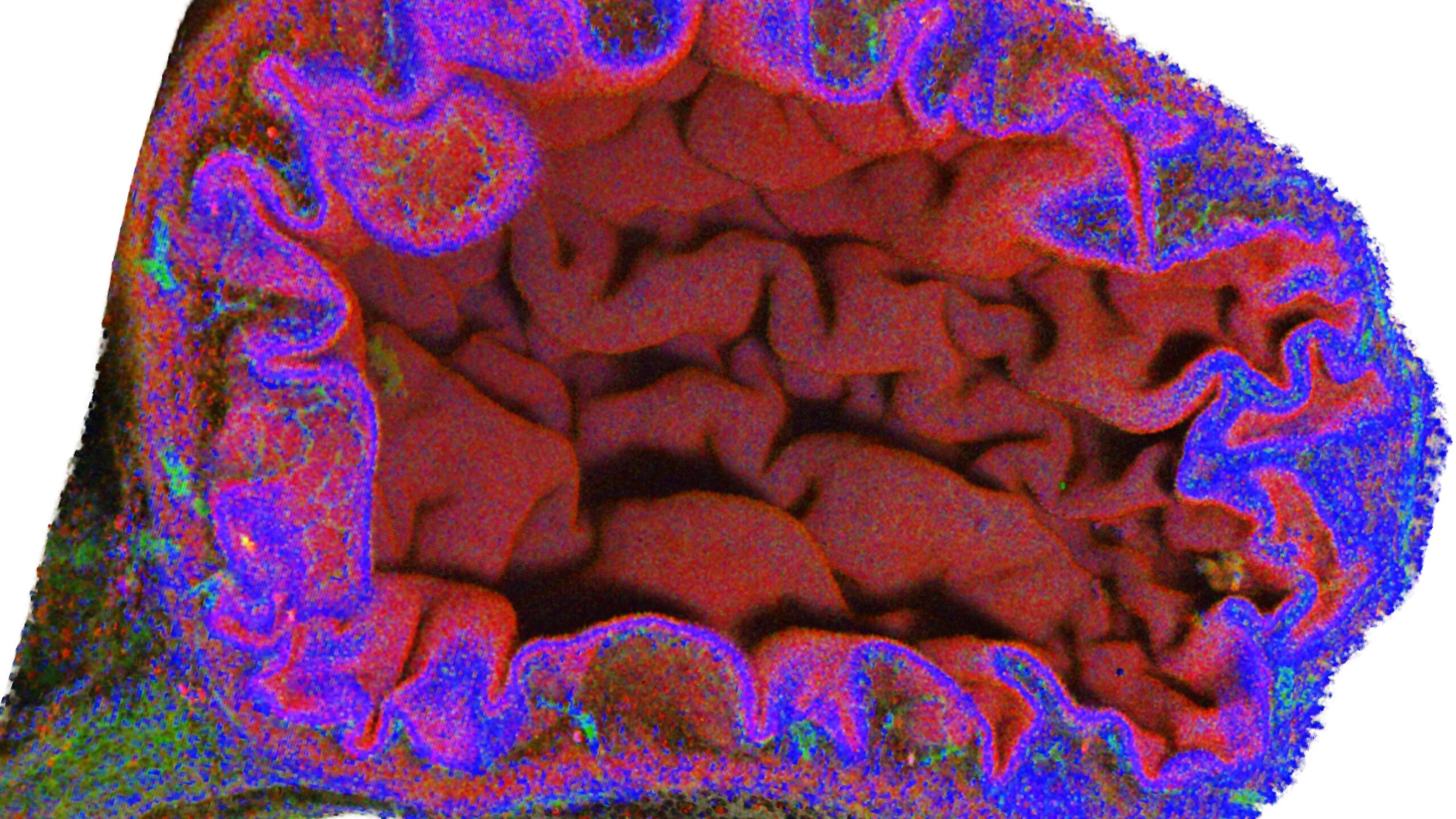
Our lab studies how cancer affects whole-body physiology, with a particular emphasis on the haematopoietic, immune and cardiovascular systems.
A prime example of cancer-host interplay is the abnormally elevated burden of cardiovascular disease that cancer patients endure. Many clinical reports are showing a correlation between cancer and cardiovascular disease. For instance, lung cancer patients have a 90% increase in the risk of coronary artery disease, and over 66% increased risk of cardiovascular disease overall in comparison to the general population, and the first cause of death of breast cancer survivors is cardiovascular disease. But we’re still lacking information on how this takes place and, most importantly, on how can we protect cancer patients and cancer survivors from this terrible burden. Understanding these critical unknowns is one of the main efforts of our laboratory.
A second example of how cancer as a systemic disease remotely affects other normal physiological processes is the changes that cancer imposes on the haematopoietic system. They are still not well understood but they are important because when the tumour remotely affects the stem and progenitor cells in the bone marrow, it can shift the production of different immune cells towards states that favour the growth and dissemination of the tumour. These same changes can also cause other problems for cancer patients, including some that will affect cardiovascular health. Understanding how this takes place to find ways to revert it is another goal of the cancer macroenvironment lab.
But cancer can affect immune cells in ways other than affecting their progenitor cells. Immune cells are exquisitely regulated because they are double-edged swords. They need to protect the host by quickly and efficiently eliminating dangers, but they also need to be careful to avoid damaging the host organism itself. In this context, we will focus primarily on neutrophils, which are the most abundant immune cells in human blood and act as first responders against many different insults. If these cells get activated in the wrong place, at the wrong time or for the wrong reasons, they can cause damage to the organism, and this plays a role in many conditions that cause a lot of human suffering, from autoimmune diseases to wound healing problems, acute lung injuries, thrombosis, myocardial infarction, stroke, and cancer. Tumours can modulate the responses of different immune cell types (they hyper-activate some and stun others) to avoid being removed, and they affect neutrophil behaviours too. We are investigating how these cancer-imposed neutrophil changes affect both cancer progression and the general welfare of cancer patients and survivors and, importantly, we are investigating therapeutic approaches to target neutrophils in cancer patients.
All these areas are highly relevant to human disease. Clinicians interested in the systemic effects of cancer, cardio-oncology, cancer immunology, cancer-related thrombosis, cancer progression, or in developing novel therapeutic options for cancer patients are welcome to discuss ideas and potential projects.
About the programme
The Francis Crick Institute invites applications for its Postdoctoral Career Development Fellowships for Clinicians, offering an exciting opportunity for postdoctoral clinicians to advance their research careers within a world-leading multidisciplinary biomedical discovery research institute.
About the Fellowships: The fellowships provide funding for one year full-time or two years part-time postdoctoral research experience in a Crick research group. The fellowships aim to:
- Foster long-term clinical links and collaborations
- Provide clinicians with a postdoctoral extension of their research experience, along with scientific networking, training and career development opportunities
- Provide a platform from which fellows may apply for external funding, such as clinician scientist fellowships, to be held at the Crick or elsewhere.
The Programme: Fellows at the Crick join a vibrant, multidisciplinary research community of over 1,000 scientists. They have full access to the Crick postdoc training programme, an extensive seminar programme, clinical academic networking opportunities, and comprehensive training and career development activities.
Funding: Successful candidates receive a salary commensurate with their current experience/ stage of training (up to but not including NHS consultant level). Research costs are also covered. Funding is available through:
- The Crick
- The Crick in partnership with the Rosetrees Trust: for translational research with the potential to benefit patients
- The Crick in partnership with Kidney Research UK: for research on earlier diagnosis, prevention or treatment of kidney disease
Who can apply: This opportunity is ideal for talented and motivated postdoctoral clinicians who are passionate about research and demonstrate outstanding potential for continuing a career in academic medicine and research. Applicants should hold (or be about to hold) a research PhD alongside their medical degree or equivalent clinical professional qualification.
Key dates:
- Fully funded fellowship application deadline: 30 April 2025
Find out more: